

Invicta MD provides comprehensive AR management services, focusing on recovering revenue from outstanding AR accounts aged over 120 days. Our proven system excels in recovering funds from accounts previously considered uncollectible. Unlike most billing companies that bundle AR recovery into their revenue cycle management packages, we offer AR recovery as a standalone service.
Started On
Review Period
Collection Increased
Revenue Increased By
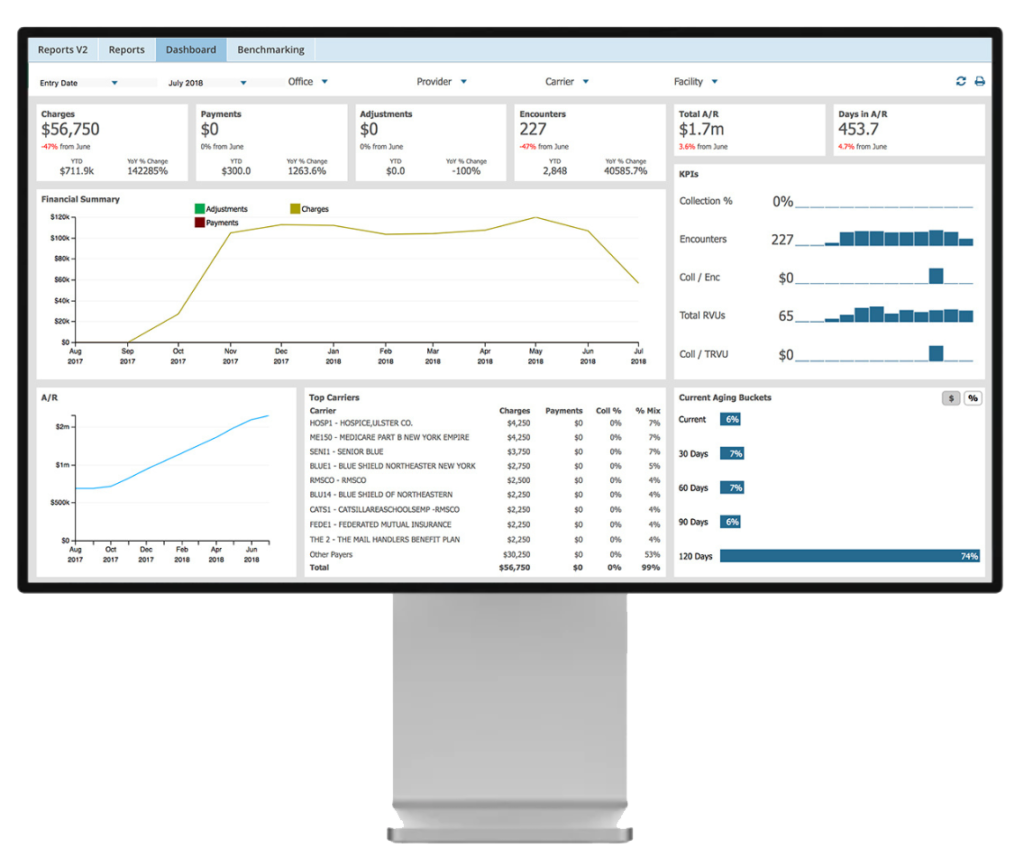
Invicta MD’s innovative claims management system ensures every claim is tracked and processed to completion, helping you secure the revenue you’re entitled to. Our methodical approach maximizes reimbursement and minimizes errors, streamlining the entire billing process for optimal results.
Invicta MD’s approach to aging AR recovery is built on years of expertise, providing a fast, effective, and tailored service.

We begin with a comprehensive review of every unresolved claim. While some may be uncollectible, we identify and pursue every opportunity for recovery. Unlike other companies that only focus on high-dollar claims, we understand the value of every claim, large or small. Our thorough process ensures no potential revenue is left behind.
We prioritize older unpaid claims to prevent them from expiring before processing. Leveraging advanced analytics, we stay ahead of payer requirements and maximize revenue recovery. Our team follows up diligently with each payer, ensuring overdue payments are collected efficiently, allowing you to focus on your practice while we manage your financial recovery.
Our team ensures no claim goes unprocessed due to errors. After correcting or clarifying any issues, we appeal rejections and denials, pushing for reconsideration from insurance or government payers. We track and analyze claim denials to identify and eliminate recurring issues, improving your overall revenue cycle.
When outstanding balances are patient-responsible, we generate clear, easy-to-understand reports and send them directly to your patients. If you prefer, we can also manage direct communication and handle phone calls and inquiries. Unlike a collection agency, we ensure a professional, transparent approach that encourages timely payments without stressing patients.

At Invicta MD, we turn unpaid claims into collected revenue. Our dedicated AR recovery team reviews ageing claims others deem “uncollectible.” We don’t shy away from old or low-value claims—instead, we tackle them efficiently, ensuring nothing is left behind. If you think a bill is beyond recovery, let Invicta MD handle it and turn it into revenue.
At Invicta MD, we assign a skilled team to investigate every unpaid claim, maximizing your revenue.
You only pay us when we successfully recover a claim. If we don’t collect, you don’t pay.
Our AR recovery team has a proven track record, recovering over 90% of claims, even those over a year old.
We handle rejections and denials with a high success rate, fixing errors and resolving complex issues.
No claim is too small. Our system recovers everything, reducing your AR.
We prioritize claims to ensure nothing expires, getting you the highest recovery possible.